If you’ve been waking up tired, struggling to focus, or your partner keeps nudging you because of loud snoring, it might not just be “poor sleep.” You could be suffering from sleep apnoea, a serious but treatable sleep disorder that affects breathing during the night.
The good news? The NHS has a clear process for identifying and treating sleep apnoea. In this post, we’ll walk you through everything UK patients need to know, from symptoms and diagnosis to the free treatment options available through the NHS.
Let’s dive in.
What Is Sleep Apnoea?
Sleep apnoea (also spelled sleep apnea) is a condition where your breathing repeatedly stops and starts during sleep. The most common type is obstructive sleep apnoea (OSA), where the throat muscles relax too much, blocking the airway.
It may sound minor, but OSA can have major consequences if left untreated, including high blood pressure, stroke, heart disease, and even type 2 diabetes. many people don’t even realise they have it. They just know they feel exhausted all the time.
Common Signs and Symptoms
Not sure if what you’re experiencing could be sleep apnoea? Here are some classic symptoms to look out for:
- Loud, persistent snoring
- Gasping, choking, or pauses in breathing during sleep
- Morning headaches or sore throat
- Feeling excessively sleepy during the day
- Trouble concentrating or remembering things
- Mood swings or irritability
Often, it’s a partner who notices the warning signs first. If any of these sound familiar, it’s worth booking an appointment with your GP to explore further.
Step 1: Visit Your NHS GP
Your first stop on the NHS pathway is a chat with your General Practitioner (GP).
At this appointment, your GP will:
- Ask about your sleep patterns and daily energy levels
- Review your medical history and lifestyle
- Possibly use the Epworth Sleepiness Scale to gauge daytime sleepiness
- Refer you to a specialist sleep clinic if sleep apnoea is suspected
Referrals are quick and straightforward. Some GPs may also recommend initial lifestyle adjustments while you wait for your sleep study.
Step 2: Sleep Study and Diagnosis
Once referred, you’ll usually be given a home sleep test kit, a simple, non-invasive way to monitor your sleep from the comfort of your own bed.

What does the test involve?
- A small monitor worn overnight
- A nasal cannula or mask to track airflow
- A pulse oximeter (clips to your finger) to monitor oxygen
- Possibly a belt across your chest to track breathing effort
You’ll return the equipment the next day, and the data will be analysed by NHS sleep specialists. In more complex cases, an in-clinic sleep study (known as polysomnography) may be arranged instead.
Step 3: Understanding Your Results
Based on your sleep data, the sleep specialist will calculate something called the Apnoea-Hypopnoea Index (AHI), the number of times you stop or restrict breathing per hour.
Here’s how they categorise it:
| AHI Score | Diagnosis |
|---|---|
| 5–14 | Mild Sleep Apnoea |
| 15–30 | Moderate Sleep Apnoea |
| 30+ | Severe Sleep Apnoea |
Even mild OSA can interfere with your health and daily life, so you’ll likely be offered some form of treatment regardless of the severity.
Step 4: NHS Sleep Apnoea Treatment Options
Once you’re diagnosed, your NHS sleep clinic will discuss next steps based on the severity of your condition.
CPAP Therapy (Continuous Positive Airway Pressure)
This is the gold standard treatment for sleep apnoea.
A CPAP machine delivers gentle air pressure through a mask to keep your airway open overnight.
Best of all? The NHS provides CPAP machines free of charge in most UK areas, along with:
- Mask fittings
- Tubing and filters
- Follow-up appointments and adjustments
If you stick with it (and most people do after the first few weeks), CPAP can dramatically improve your sleep and health.
Lifestyle Adjustments
Alongside any device-based treatment, your doctor will likely recommend some lifestyle changes, especially if your apnoea is mild or linked to excess weight.
Helpful tips include:
- Losing weight (even a small amount can help)
- Avoiding alcohol or sedatives at night
- Sleeping on your side, not your back
- Quitting smoking
- Keeping your nasal passages clear
These changes alone can significantly reduce symptoms for many people.
Dental Devices (MADs)
If CPAP isn’t right for you, or if your case is mild to moderate, you may be offered a Mandibular Advancement Device (MAD).
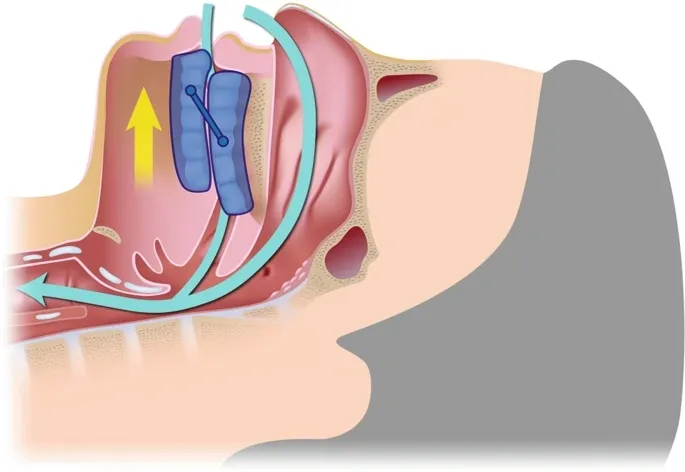
These custom-made dental devices gently move your lower jaw forward to help keep your airway open during sleep.
They aren’t always available through the NHS, but some Trusts do offer them. Alternatively, you can purchase one privately (expect to pay £200–£800).
Surgical Options (Rare)
In certain rare cases, typically where there are physical obstructions like large tonsils or nasal blockages surgery may be considered.
You’ll need a referral to an ENT (Ear, Nose, and Throat) specialist or oral/maxillofacial team. Surgery is usually only offered if other treatments fail or aren’t suitable.
Does NHS Treatment Cost Anything?
No! If you’re going through the NHS system:
- Sleep studies are free
- CPAP therapy and supplies are provided at no cost
- Follow-up care and replacements are handled through your local sleep clinic
This makes the sleep apnea NHS pathway one of the most accessible and effective systems in the world for treating sleep disorders.
How Long Does It Take?
Every NHS Trust operates slightly differently, but here’s a general idea of the timeline:
- Referral to sleep clinic: 4–12 weeks (depending on location)
- Testing and results: 2–3 weeks
- Treatment (CPAP or other): Usually starts shortly after diagnosis
Waiting times are improving, and you can also choose to go private for faster diagnosis if desired.
Private vs NHS Sleep Apnoea Care: What’s the Difference?
Going private can give you:
- Faster access to sleep testing and diagnosis
- More customisation in mask or device choice
- One-on-one consultations and long-term support
However, you can still switch to the NHS later if your private provider shares the results with your GP.
For most people, NHS diagnosis and treatment is free, reliable, and more than sufficient, especially if you’re eligible for CPAP.
Final Thoughts
If you’re feeling constantly tired, foggy, or have been told you snore like a chainsaw, don’t ignore it.
Sleep apnoea is common, treatable, and potentially life-threatening if left undiagnosed. The NHS offers a well-structured, evidence-based approach to diagnosis and treatment, without the price tag.