Imagine your body suffocating while you sleep. You wake up gasping for air, your heart racing. Yet, you don’t remember any of it in the morning. This isn’t a horror film; it’s a nightly reality for millions with obstructive sleep apnoea (OSA), often without their awareness. But can sleep apnea kill you? The potential dangers of untreated sleep apnea are serious and should not be ignored.
OSA is one of the most underdiagnosed and dangerous sleep disorders. While it may begin with nothing more than loud snoring and daytime tiredness, its long-term effects on the heart and brain can be deadly.
Understanding Obstructive Sleep Apnoea
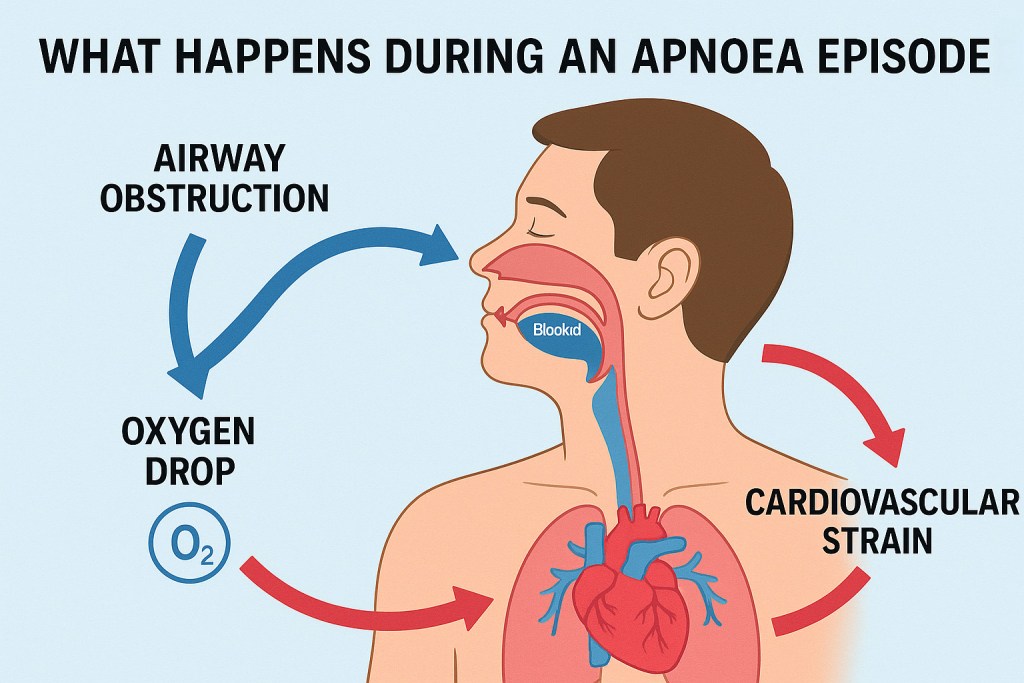
Obstructive sleep apnoea occurs when the muscles at the back of the throat relax too much during sleep, causing the airway to collapse. This blocks airflow, reducing oxygen levels and forcing the brain to wake up partially to reopen the airway. These events can happen anywhere from a few times to hundreds of times a night.
People with moderate to severe OSA often wake up feeling unrested despite sleeping for 7 to 8 hours. Symptoms like daytime fatigue, difficulty concentrating, morning headaches, or mood changes are common. But beneath these relatively minor symptoms, serious damage may be unfolding inside the body.
The Hidden Cardiovascular Toll
Each time breathing stops, the oxygen level in the blood drops. This drop triggers the brain to send emergency signals that increase heart rate and blood pressure. This repeated cycle — oxygen deprivation followed by a surge of adrenaline, creates a state of chronic stress in the body.
Over time, these nightly stress responses damage the blood vessels, promote inflammation, and lead to high blood pressure. The heart, constantly jolted awake from its normal rhythm, becomes strained and overworked. These effects increase the risk of several life-threatening conditions including:
- Hypertension
- Coronary artery disease
- Heart failure
- Stroke
- Sudden cardiac death
The Link to Sudden Cardiac Death
Sudden cardiac death (SCD) refers to an unexpected death due to cardiac causes, occurring within one hour of the onset of symptoms. In many cases, there are no early warning signs. A person may go to sleep seemingly healthy and never wake up.
| Health Risk | Description | Supporting Study / Statistic |
|---|---|---|
| Hypertension | Increased sympathetic activity leads to sustained high blood pressure. | Peppard et al., NEJM 2000: 2-3x increased risk |
| Stroke | OSA increases risk of ischemic stroke due to intermittent hypoxia. | Yaggi et al., NEJM 2005: 2x increased risk |
| Sudden Cardiac Death (SCD) | Risk increases by 2.5 times, especially during sleep. | Gami et al., NEJM 2005: 2.57x risk during sleep |
| Atrial Fibrillation (AFib) | AFib incidence is 4 times higher in OSA patients. | Gami et al., Circulation 2004: 4x risk of AFib |
| Type 2 Diabetes | Intermittent hypoxia contributes to insulin resistance. | Punjabi et al., AJRCCM 2004: Elevated fasting glucose levels |
| Heart Failure | Left ventricular dysfunction and fluid retention are common. | Redline et al., Circulation 2010: Higher rates of HF |
Over the past decade, multiple large-scale studies have revealed a strong association between untreated obstructive sleep apnoea and sudden cardiac death. One of the most influential studies, published in the journal Sleep in 2013, followed over 10,000 adults and found that individuals with severe untreated OSA had a 2.5 times greater risk of sudden cardiac death than those without OSA (source).
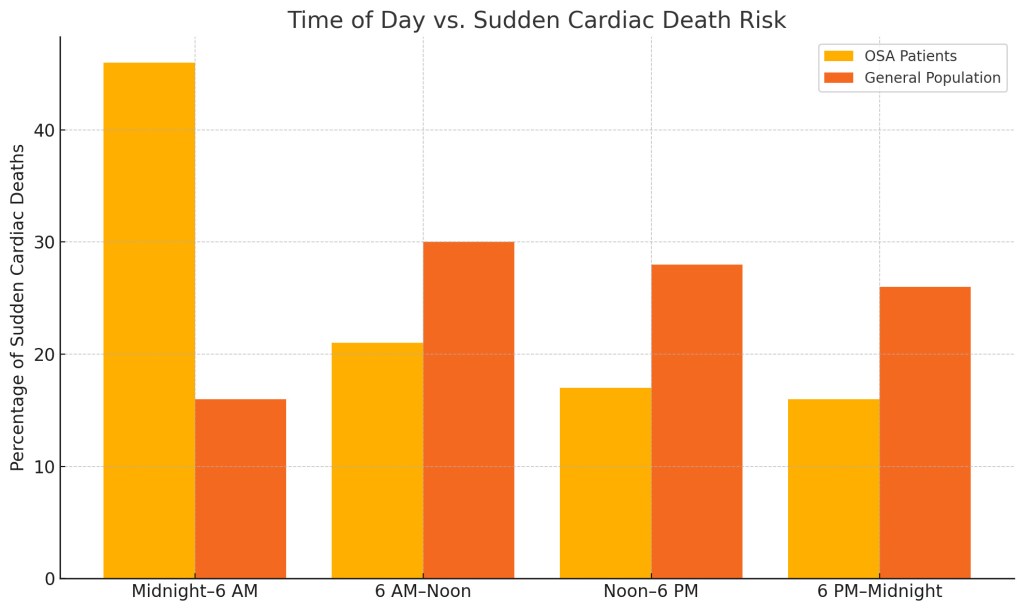
Another key finding is that deaths in individuals with sleep apnoea are more likely to occur during the night. While sudden cardiac death in the general population tends to peak in the early morning hours (typically between 6 a.m. and noon), people with OSA are more likely to die between midnight and 6 a.m. This inversion of the usual pattern highlights the role of apnoea-related events, especially oxygen desaturation and arrhythmias — as critical triggers during sleep (source).
Atrial Fibrillation and Irregular Heartbeats
One of the clearest pathways from obstructive sleep apnoea to sudden cardiac death is through arrhythmias, which are abnormal heart rhythms that disrupt the heart’s normal electrical signals. Episodes of apnoea cause dramatic fluctuations in oxygen and carbon dioxide levels during sleep, placing acute stress on the cardiovascular system.
Atrial fibrillation (AF), the most common type of arrhythmia, is significantly more prevalent in people with OSA. Research published in the Journal of the American College of Cardiology has shown that up to 50 percent of patients with AF also have undiagnosed sleep apnoea, particularly among older adults and those with preexisting heart conditions (source).
If left untreated, AF increases the risk of stroke and heart failure. Moreover, OSA undermines the effectiveness of common AF treatments like catheter ablation and medication. A review from the American Heart Association emphasizes that treating sleep apnoea in tandem with AF significantly improves long-term outcomes and reduces recurrence rates. As a result, many cardiologists now routinely recommend sleep studies for patients diagnosed with atrial fibrillation.
Real-Life Impact: Case Examples ( Sleep Apnea Nearly Killed Michael)
Consider the case of 42-year-old Michael, a New Jersey firefighter. For months, he had been waking up with pounding headaches and feeling exhausted despite getting full nights of sleep. His wife noticed he would stop breathing repeatedly during the night.

After a sleep study, he was diagnosed with severe OSA, experiencing more than 70 breathing interruptions per hour. His cardiologist was alarmed to discover early signs of cardiac remodeling and irregular heartbeat. Once Michael began using CPAP therapy, his heart rate stabilized and his blood pressure dropped to a healthy level, aligning with findings from studies that show CPAP significantly reduces cardiovascular risk.
Another example is Angela, a 55-year-old teacher who suffered a stroke in her sleep. Doctors later found she had undiagnosed OSA, which had gone unnoticed for years. Angela had always assumed her snoring and fatigue were just part of getting older. This mirrors research showing that sleep apnoea increases stroke risk independently of other factors.
These cases are not rare. Stories like these are becoming increasingly common as awareness of sleep apnoea grows.
Sleep Apnoea and Other Health Risks
Beyond the heart, OSA affects nearly every major system in the body.
- Stroke: OSA triples the risk of stroke. The nightly swings in blood pressure and oxygen strain the brain’s blood vessels, making them more likely to rupture or clot.
- Metabolic Disorders: People with sleep apnoea are more likely to develop type 2 diabetes and metabolic syndrome, even if they are not overweight. The inflammation and insulin resistance caused by poor sleep play a major role.
- Cognitive Decline: Chronic sleep fragmentation from apnoea is linked to memory loss, depression, and even early Alzheimer’s disease.
The Role of CPAP Therapy
The good news is that sleep apnoea is treatable. The gold standard of treatment is CPAP therapy — short for Continuous Positive Airway Pressure. A CPAP machine uses a gentle stream of air to keep the airway open during sleep.
Studies have shown that regular CPAP use:
- Reduces apnoea events to nearly zero
- Lowers blood pressure
- Improves heart function
- Reduces the risk of stroke and heart attacks
- Enhances mood, memory, and daytime energy
Patients often report dramatic improvements within just a few days of starting treatment.
However, CPAP is not a cure. It only works if it is used consistently every night. That is why comfort, support, and education are key to long-term success.
Alternative Treatments
For people who cannot tolerate CPAP, other options include:
- Oral appliances: These custom-fit devices reposition the jaw to keep the airway open.
- Surgical procedures: In some cases, surgery to remove excess tissue in the airway is recommended.
- Inspire therapy: An implantable device that stimulates the airway muscles during sleep.
In addition, certain lifestyle adjustments can help improve sleep quality and reduce apnoea episodes. These include weight loss, reducing alcohol use, quitting smoking, and changing sleep position. Even your mattress and sleep posture may play a role in worsening or relieving symptoms of sleep apnoea. Choosing the right mattress can support proper airway alignment and reduce positional apnoea. For more on this, see “Is Your Mattress Worsening Your Sleep Apnea?”.
Improving Sleep Quality and Addressing Comorbidities
Managing obstructive sleep apnoea effectively often requires more than just treating airway obstruction. Many patients with OSA also struggle with insomnia, anxiety, or poor sleep habits that reduce sleep quality even when apnoea events are controlled.
Optimizing your sleep environment and addressing these coexisting issues can significantly improve both treatment adherence and how rested you feel. Practicing better sleep hygiene, reducing screen time before bed, and learning to calm an overactive mind are all part of a holistic approach.
For those struggling with insomnia alongside OSA, consider this science-backed guide to managing insomnia without medication. It covers evidence-based techniques such as CBT-I, relaxation methods, and other holistic strategies that complement OSA treatment.
Public Health and Economic Impact
Sleep apnoea is not just a personal health issue. It is also a growing public health concern.
Untreated OSA is associated with increased healthcare costs due to frequent doctor visits, hospitalizations, and complications like stroke and heart failure. It also contributes to lost productivity, workplace accidents, and drowsy driving incidents.
According to the American Academy of Sleep Medicine, undiagnosed OSA costs the U.S. economy more than $150 billion per year.
Take Action: What You Should Do
If you suspect you or a loved one has sleep apnoea, do not wait. Talk to your primary care doctor or a sleep specialist. A simple overnight sleep study can diagnose the condition.
Look out for these warning signs:
- Loud snoring
- Pauses in breathing during sleep
- Gasping or choking sounds at night
- Morning headaches
- Excessive daytime sleepiness
- Trouble concentrating or memory problems
- High blood pressure that is hard to control
Sleep apnoea is not a condition to ignore or push aside. Early diagnosis and consistent treatment can save your life, literally.
Conclusion: Silence Can Be Deadly
Sleep apnoea may be silent, but its effects are anything but harmless. It puts immense pressure on the heart, disrupts your body’s natural rhythms, and dramatically increases the risk of sudden death, particularly in the quiet hours of the night.
Fortunately, with greater awareness, better diagnostics, and effective treatments like CPAP, we now have the tools to fight back. Do not sleep on your symptoms. If something feels off, take it seriously. It might be the first step toward protecting your heart, your health, and your future.